Jon Brock
www.crackingtheenigma.blogspot.com/
Some cases of autism are obvious. Anyone who knew anything about autism would agree that the child or adult in question was autistic. Other cases are less clear cut. Indeed, the term “autism spectrum” implies the existence of a continuum that fades gradually into what we think of as the “normal” population.
Somewhere a line has to be drawn and where exactly we choose to draw that line defines what we mean by autism. It determines who is eligible to take part in autism-related research and this in turn influences the development of theories of autism. Eventually, this feeds back to our evolving definitions and cut-offs for autism. Most importantly when it comes to immediate real-world consequences, the diagnostic boundaries specify who is labeled “autistic” and, ultimately, who gains access to interventions and support.
In the absence of reliable biological markers or break points in the continuum, diagnoses are made by checklist. Tick enough boxes and you get a diagnosis of “autistic disorder” or “Asperger’s disorder”. Tick fewer boxes or the “wrong” combination of boxes and you’re not considered autistic. You may, however, qualify for the mysterious diagnosis of PDD-NOS – “Pervasive Developmental Disorder -Not Otherwise Specified”.
Defining PDD-NOS
“Pervasive Developmental Disorder” is an umbrella term covering five diagnoses:
- Autistic disorder
- Asperger’s syndrome
- Rett syndrome
- Childhood disintegrative disorder
- PDD-NOS
As the name suggests, PDD-NOS is generally thought of as a residual category for people who have a pervasive developmental disorder but don’t quite fit into the other more specific categories. However, this all gets a bit circular because “pervasive developmental disorder” is defined only in terms of its constituent diagnoses. You’ve got a pervasive developmental disorder if you have any of the five diagnoses above (including PDD-NOS), and you’ve got PDD-NOS if you don’t have the other four.
In practice, PDD-NOS is defined along the same lines as autism but with less strict cut-offs. Current autism diagnostic criteria require evidence of difficulties in each of three “domains” – the famous autistic triad of:
- social impairments
- communication impairments
- repetitive and stereotyped behaviours (RSBs for short).
The 1994 version of the diagnostic rules allowed a PDD-NOS diagnosis to be given to anyone with significant impairment in any one of the three domains.
However, the most recent revision, published in 2000, is much more restrictive. PDD-NOS is currently defined as:
“a severe and persistent impairment in the development of reciprocal social interaction associated with impairment in either verbal or nonverbal communication skills or with the presence of stereotyped behavior, interests and activities”
In other words, there has to be evidence of impairment in exactly two domains and one of these has to be the social domain.
Confused? You ought to be.
PDD-NOS and DSM 5
In 2013, the diagnostic rules are set to change yet again. One of the proposals for the new set of rules, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM 5), is to do away with the current distinction between autism, Asperger’s, and PDD-NOS, replacing them with a single super-category of “Autism Spectrum Disorders“.
While there has been heated debate about the abolition of the Asperger’s diagnosis, there appears to be little opposition to the demise of PDD-NOS. It’s not hard to see why. The term itself is unwieldy, suggesting diagnostic uncertainty. And there’s no real sense of a PDD-NOS identity as there is for Asperger syndrome.
An important question, however, is what will happen to people who would currently be diagnosed with PDD-NOS? In a study, published recently in the journal, Autism Research, William Mandy and colleagues at University College London set out to address precisely this question.
Specifying PDD-NOS
The study centred on the Developmental, Dimensional and Diagnostic Interview (known as the 3Di), a semi-structured interview, which provides scales for the three autism domains (social, communication, RSBs) as well as a number of other clinically relevant scales such as auditory sensitivity, motor impairment, and sleep difficulties.
The 3Di was administered to parents of 256 children who had been referred for assessment. Based on the parents’ responses, the researchers were able to identify 66 kids who met criteria for PDD-NOS according to the current rules. In other words, these kids were above the diagnostic threshold on the social scale and either the communication or the RSB scale. The remaining kids in their sample were above the threshold on all three scales and so were diagnosed with autistic disorder or Asperger’92s disorder (depending on their history of language development).
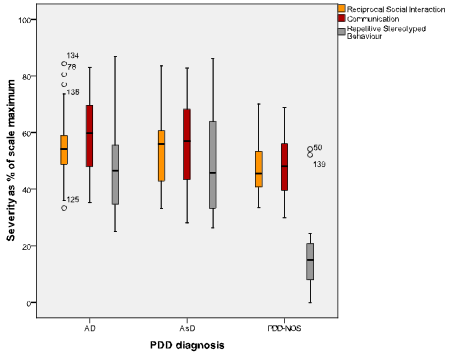
The graph below shows the scores of the kids in the three diagnostic groups on each of the three main scales. Compared with children meeting criteria for autistic disorder or Asperger’s disorder, the kids with PDD-NOS on average had lower scores (less impairment) on all three diagnostic scales. They also scored lower on the scales for auditory sensitivity, visuo-spatial impairment, and feeding difficulties (not shown in the graph).
As you can see in the far right column, group differences were particularly marked on the RSB scale. Indeed, the authors found that only two of the 66 PDD-NOS kids had clinically significant RSBs and both of these children were very close to also meeting the communication criterion, which would have given them a full autism diagnosis. The remaining 64 PDD-NOS kids fell well short of criteria for RSBs and achieved their PDD-NOS diagnosis by virtue of having both social and communication difficulties.
The authors acknowledge that this isn’t a huge sample and that kids weren’t selected at random from the community so it might not give a totally accurate picture of the prevalence of the different diagnostic categories. However, their results suggest that what we currently term PDD-NOS should not be thought of as simply a milder form of autism. Nor is it, as the name suggests, merely a rag-bag miscellaneous category for kids whose difficulties can’t quite be pinned down. Rather, the PDD-NOS label appears to broadly correspond to those individuals facing social and communication difficulties in the absence of the RSBs that characterize autism and Asperger’s.
Implications for DSM 5
As Mandy et al. point out, their findings suggest a potential unforeseen consequence of the proposed changes to diagnostic criteria in DSM 5.
To receive a diagnosis of “Autism Spectrum Disorder” (which is supposed to replace autism, Asperger’s and PDD-NOS), an individual will have to show evidence of both:
- social and communication impairment (these two domains will be merged)
- repetitive and stereotyped behaviors (RSBs)
Under these rules, 64 of the 66 children in the PDD-NOS group would not meet the criteria for Autism Spectrum Disorder. To the extent that Mandy et al.’s data are at all representative, this suggests that the overwhelming majority of people who currently meet criteria for PDD-NOS would not be considered autistic under DSM 5 and may not receive any form of diagnosis.
There is certainly a case to be made that children are being over-diagnosed and that the boundaries for autism-related disorders should be brought in. However, as Mandy et al. point out, there is also a real danger that individuals with severe social and communication difficulties would be excluded from support and interventions designed to improve their social and communication skills. All because they don’t also have RSBs.
Social Communication Disorder
In response to Mandy et al., Prof Francesca Happé, a member of the DSM-5 working group, had the following to say:
“Recently, Mandy et al. raised concerns that many children currently receiving [a PDD-NOS] diagnosis will not meet proposed DSM-5 criteria for ASD because of a lack of restricted / repetitive behaviour. For these children, the proposed new neurodevelopmental diagnostic category of social communication disorder will be relevant. This diagnosis, it is hoped, will more clearly and accurately capture the pattern of impaired social and communication abilities seen in the largest subgroup now labeled PDD-NOS”.
On the DSM 5 website, the new disorder is defined more formally:
“Social Communication Disorder (SCD) is an impairment of pragmatics and is diagnosed based on difficulty in the social uses of verbal and nonverbal communication in naturalistic contexts, which affects the development of social relationships and discourse comprehension and cannot be explained by low abilities in the domains of word structure and grammar or general cognitive ability.”
Effectively, SCD seems to be official recognition for what researchers and practitioners have previously referred to as “Pragmatic Language Impairment” rather than a replacement for PDD-NOS. The emphasis is very much on the communication side of things, particularly conversation skills, with a suggestion that social difficulties are a secondary consequence of impaired communication. That’s my interpretation at least.
As Happé suggests, it seems likely that many people who currently find a place in the PDD-NOS “pigeon hole” would meet the SCD criteria. However, I’m not sure that the criteria necessarily capture the extent of the issues they face. As Will Mandy commented:
“Our clinical experience is that children with PDD-NOS (i.e. mainly individuals with severe autistic social-communication difficulties, but without high levels of repetitive and stereotyped behaviours) are similar to those with a full autism diagnosis in terms of their functional impairment.”
What is autism?
Although Mandy et al.’s study focused on PDD-NOS, it also raises some wider philosophical questions about what we actually mean by “autism” or “autism spectrum disorders”. In particular, how do we determine what counts as a defining feature of autism?
Up until the early 1970s, language impairment was seen as one of the major defining features of autism. Indeed, researchers such as Michael Rutter argued that autism was essentially a severe form of language impairment. This theory was abandoned, however, when it became clear that there were some individuals who had the social impairments associated with autism, despite having very good language skills. Gradually, the diagnostic criteria were relaxed and today language impairment is no longer considered a necessary criterion.
Mandy et al.’s study seems to present an analogous situation with respect to repetitive and stereotyped behaviours (RSBs). As with language impairment, RSBs have long been considered a defining feature of autism. And, as with language impairment, it now appears to be the case that a substantial group of individuals exhibit social impairments without exhibiting RSBs. This begs the question of why RSBs should continue to be considered a defining characteristic of autism when language impairment is not.
Thinking outside the diagnostic box
In essence, autism is whatever we say it is. Although we might like to think of it as a natural kind – an objectively discrete entity that falls out of nature, we are, as Prof Happé delicately put it, trying to “carve meatloaf at the joints”. DSM 5 isn’t going to change that, even if it changes where those cuts are placed.
Given our current state of ignorance, there is little practical alternative to this approach to diagnosis at this time. But it’s still important to constantly remind ourselves that the lines between autism and not-autism are, to a certain extent, arbitrary. Indeed, researchers like myself will have to learn to think outside the prevailing diagnostic boxes if we ever hope to understand autism’s place in the human spectrum.
References:
Happé F (2011). Criteria, Categories, and Continua: Autism and Related Disorders in DSM-5. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 540-542.
Mandy W, Charman T, Gilmour J, & Skuse D (2011). Toward specifying pervasive developmental disorder-not otherwise specified. Autism Research, 4, 121-131.}